786 471 8955 (Call or Text)
786 524 8204 (Fax)
Islon Woolf MD
About
Philosophy
I am an internist who believes that medicine is an intellectual discipline, not a product to be sold. My practice is designed to help patients filter through the healthcare noise and separate what is true from what we hope is true.
Training
I was born in Johannesburg, South Africa and grew up in Toronto, Canada. My training began at the University of Toronto, where I pursued an undergraduate degree in Biology and Physics, and in 1989, gained an early acceptance to their highly ranked medical school.
Post-Grad Training
In 1993, I moved to the United States to complete my post-grad training. This included an Internal Medicine internship at the University of Southern California, an Internal Medicine Residency at the Mayo Clinic, and a Chief Residency at the Cleveland Clinic. I am board certified in Internal Medicine and a Fellow of the American College of Physicians (FACP).
25 years of Concierge Medicine Experience
I began practice in 1997, and quickly discovered that I had a passion for working closely with patients and showing them how to apply critical thinking to their health. In 2002, to be able to have the time to practice this way, I became one of the first concierge doctors in the city.

Concierge Medicine
About
The 15-Minute Appointment
Due to the constraints of insurance, the average appointment with your doctor lasts fewer than fifteen minutes. This is particularly problematic in primary care where we must oversee the entirety of your health. Tasks like coordinating care, promoting prevention, and solving complex medical problems demand far more time.
Fewer Patients, More Time
For those willing to invest more into their health, concierge medicine offers an effective solution. The basic principle of every concierge practice is the same: patients pay a fee so the doctor sees fewer patients and has more time. My practice, for example, is capped at three hundred patients, and I see fewer than three patients per day.
5 Ways
More Time Leads to Better Outcomes
5
More Time
Better Outcomes
Access
1
Access to healthcare means timely visits and seamless communications with me, my team, and the network of specialists I've built over the last 25 years. Improved access leads to early intervention, fewer errors, and better outcomes.
Decision-readiness
2
Although decision-making is the cornerstone of healthcare, healthcare professionals are plagued by decision fatigue and burnout. With fewer than three patients per day, our practice is shielded from this. We are always decision-ready.
Continuity of Care
3
Your health is complex and dynamic. Healthcare systems are fragmented and impersonal. You need a stable, well-established practice to coordinate, document, and ensure follow-through. This is continuity of care, and a major determinant of good outcomes.
Efficiency
4
Most primary care doctors create inefficiencies by requiring office visits, and then limited by time, refer you to specialists. My mandate is to solve your problems, regardless of time, location, or how we communicate.
Accuracy
5
Accuracy in diagnosis and treatment depends on two things: mastering the specific details of your case and applying the most current medical research. My team and I have the time so your care is guided by up-to-date data, not habit.
3
Critical Thinking in medicine
About
Concierge Medicine is an Amplifier
While concierge medicine - having a doctor with more time - is necessary for good healthcare, it's by no means sufficient. Time is simply an amplifier. If a doctor’s philosophy is flawed, more time just gives more room to carry out bad ideas. Before joining a practice, you should determine the doctor's philosophy.
Incentivized to Lower Evidence Standards
Unfortunately, doctors have a powerful incentive to lower their evidence standards. By requiring only an anecdote or animal study as proof, they can make 'wellness', 'longevity', and even 'miracle cure' claims. This not only builds a following for them, it creates a platform to 'upsell' tests, supplements, and procedures.
The Dilemma of Low Evidence Standards
A serious problem occurs when evidence standards are lowered: weak evidence can be found for every claim, so every claim can be made to look true. The result: total confusion. Thousands of claims about what makes you healthy, no two doctors making the same set of claims, and claims that just flatly contradict one another - one doctor calls meat a superfood, while another calls it a toxin.
Filtering the Noise
This multitude of contradictory claims begs the question: How do you determine which of these claims, if any, are actually true? This is Critical Thinking in medicine. It is the central philosophy of my practice: to help you filter the noise, question the evidence, and empower you to evaluate medical claims for yourself.
Principles of
Critical Thinking in Medicine

6
Principles of
Critical Thinking in Medicine
Patient empowerment
1
Patients are unable to assess healthcare for themselves and left to trust experts. Unfortunately, experts are prone to bias and harbor conflicts of interest. As a result, good healthcare is not about more healthcare, it's about learning how to evaluate healthcare for yourself.
Evaluation of claims
2
Evaluating a medical claim is not as difficult as it seems. We teach you how to gather and categorize the evidence for a claim, and then rank it with the medical hierarchy of evidence. This process can be applied to any claim you encounter.
Addressing bias
3
Bias when evaluating claims is unavoidable. Practitioners carry conflicts of interest, specialists favor their own specialty, the media wants more clicks, and patients want to feel better. Our practice is engineered to avoid bias and teach you how to identify bias in yourself and in others.
Comprehensive analysis
4
There are many treatment options outside of pharmaceuticals and surgery. There are many philosophies of practice outside of science-based medicine. You need to learn all of your options in order to make informed decisions.
Shared decision-making
5
Most decisions in healthcare are not black or white: the evidence is weak, each patient responds differently, and each patient has a different tolerance for risk. The best medical decisions are made when you and I work together to incorporate these uncertainties and your values and preferences.
Lifelong learning
6
For the critical thinker, medical school marks only the beginning. A lifetime of learning teaches us that knowledge is incomplete, becomes quickly outdated, and frequently refuted. It cultivates the critical thinker's most valuable asset: intellectual humility.
Critical Thinking in Medicine
Blog
Patients are Vulnerable to False Claims
Healthcare is filled with thousands of claims, most of which are untrue. Unfortunately, the technical complexity of medical science leads many patients to believe they are incapable of evaluating claims for themselves. They rely on others - who are often biased - to do it for them, leaving them vulnerable.
Evaluating Claims for Yourself
Fortunately, evaluating a medical claim is not as difficult as it seems. In reality, it can be simplified into a process that can be applied to any claim. The goal of this blog is to teach you this process so you can move past biased advice and evaluate claims for yourself.
The Process
-
The strength of any claim is proportional to the strength of evidence that supports it.
-
Evidence in medicine falls into just a few well-defined categories.
-
Each category is predictably reliable and can be ranked into a hierarchy. (see below)
-
To evaluate a claim: search for the evidence, identify the category it belongs to; the higher the category, the more likely the claim is true.
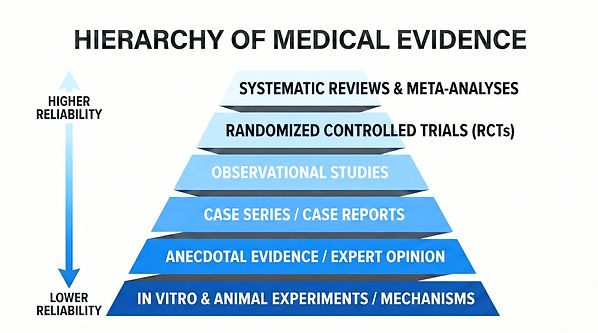
Evidence that supports every claim supports no claim
The hierarchy of medical evidence is pyramid-shaped, widest at the bottom. Categories here are not only unreliable, but because they are cheap and easy to produce, they are plentiful. There's an anecdote or rat study for EVERY claim. This is why the health and wellness industry loves them. However, the abundance of evidence in these categories renders them nearly useless. Evidence that supports every claim supports no claim.
Value the Process, Not the Outcome
The health and wellness industry are not the only ones that want their claims to be true. We all want to live long and healthy, and we tend to make exceptions for outcomes we desire. OUR anecdotes and OUR rat studies ARE reliable. Critical thinking is not just about bias in others, it's about bias in ourselves. Of all the skills in critical thinking, learning to value the process over of the desired outcome, is the most challenging.
Our Most Recent Posts
and Sign-up Form